Kidney transplantation is widely recognized as the best treatment for people with end-stage kidney disease. It offers longer survival, better quality of life, and freedom from long-term dialysis. However, for many patients, getting a kidney transplant is not just about finding a donor—it is about overcoming the body’s own immune response. For some individuals, the immune system becomes a major barrier. These patients are known as sensitized kidney transplant candidates, and for them, plasmapheresis has emerged as a life-changing solution.
Every person has antibodies—protective proteins produced by the immune system to fight infections. This is completely normal. But in kidney transplantation, doctors focus on a specific type called anti-HLA antibodies (Human Leukocyte Antibodies).
These antibodies do not protect against infections. Instead, they can recognize and attack tissues from another person, including a transplanted kidney. Anti-HLA antibodies may develop after:
In many patients, these antibodies are present at low levels and do not interfere with transplantation. However, some individuals develop high levels or a broad range of anti-HLA antibodies, making their immune system highly reactive to most donor kidneys.
Such patients are called highly sensitized kidney transplant patients. They often face:
This immune sensitization is one of the biggest challenges in modern transplant medicine.
Plasmapheresis, also known as plasma exchange, is a medical procedure that removes unwanted antibodies from the bloodstream. It is commonly used as part of desensitization therapy before kidney transplantation, especially in highly sensitized patients.
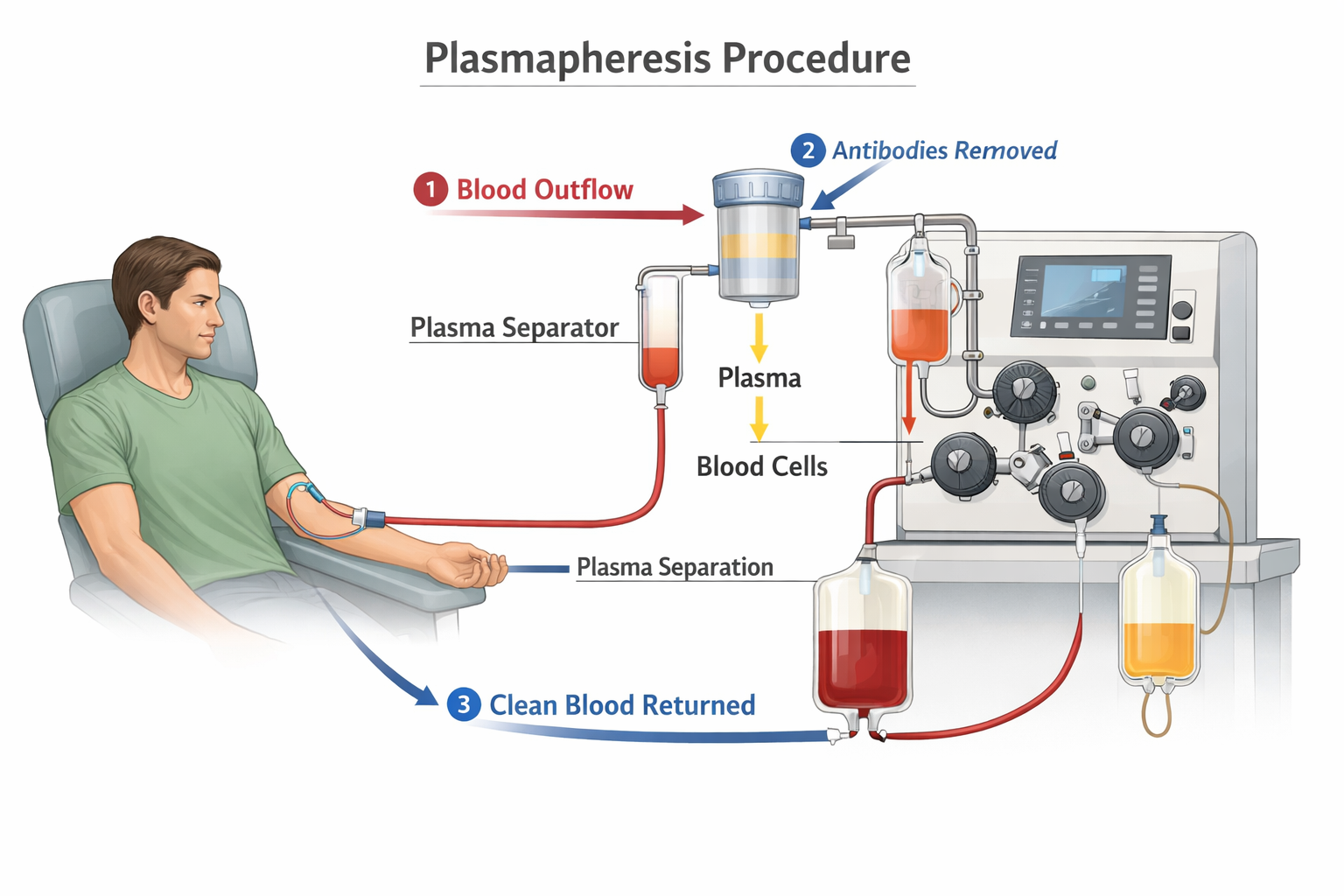
During plasmapheresis:
By lowering the concentration of donor-reactive antibodies, plasmapheresis reduces the risk of antibody-mediated rejection and improves the chances of a successful kidney transplant.
Plasmapheresis is rarely used alone; instead, it is usually part of a comprehensive desensitization protocol, which may include

This combined approach helps “retrain” the immune system, allowing patients who were previously considered incompatible to safely receive a kidney transplant.
Without desensitization, highly sensitized patients may, therefore, remain on dialysis for years or may never receive a transplant. Studies have shown that plasmapheresis-based desensitization can:
For many individuals, plasmapheresis has, therefore, transformed kidney transplantation from a distant hope into a realistic possibility.
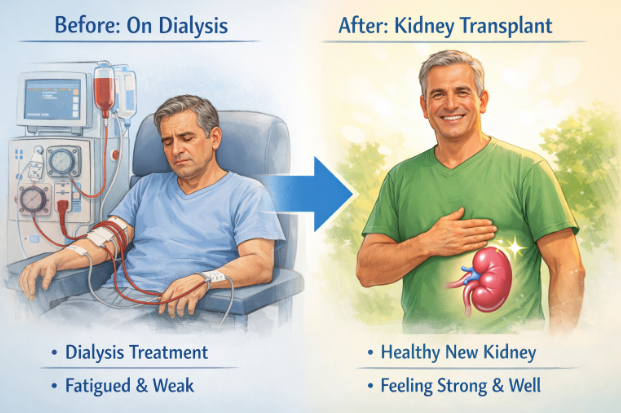
Plasmapheresis does not eliminate the immune system—it carefully adjusts it. By reducing unwanted antibodies at the right time, this therapy opens a crucial window for transplantation and gives highly sensitized patients a second chance at life.
In the evolving field of kidney transplantation, plasmapheresis stands as a powerful example of how science, precision medicine, and compassionate care come together to overcome even the toughest immunological barriers.