- 2285
- 2
Managing and Living with Irritable Bowel Syndrome (IBS)

Irritable Bowel Syndrome (IBS),is a common gastrointestinal disorder affecting millions of individuals worldwide. IBS is a chronic condition characterized by a range of digestive symptoms, such as abdominal pain, bloating, and irregular bowel movements. Despite its prevalence, IBS remains a misunderstood and often undiagnosed condition, leading to considerable discomfort and reduced quality of life for those affected. In this blog, we will delve into the intricacies of IBS, exploring its potential causes, symptoms, diagnosis, and available management strategies. By shedding light on this complex condition, we hope to empower individuals with the knowledge and tools necessary to navigate their IBS journey effectively and find relief.
You can call IBS by different names:
- spastic colon,
- irritable colon,
- mucous colitis, and
- spastic colitis.
IBS is a separate condition from inflammatory bowel disease and isn’t related to other bowel conditions.
What are the symptoms of IBS?
The most common symptoms of irritable bowel syndrome (IBS) are recurrent abdominal pain on average at least a day a week in the last 3 months, associated with two or more of the following criteria (Rome IV criteria):
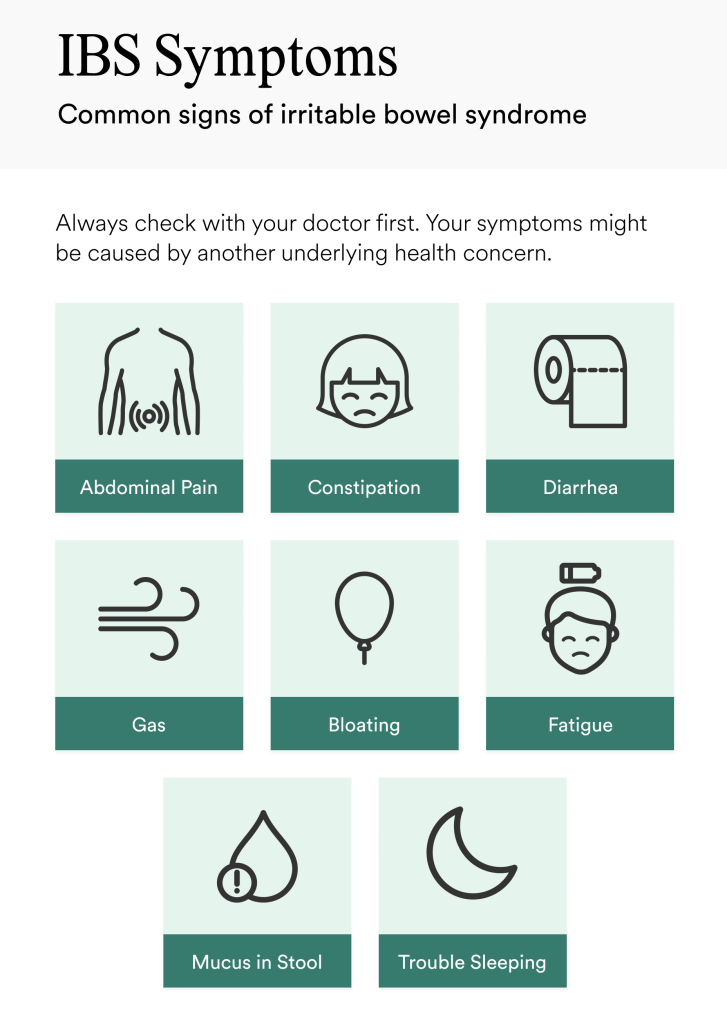
- Related to defecation
- Associated with a change in the frequency of stool
- Associated with a change in the form (appearance) of stool
The other symptoms of IBS that you may suffer with
- Bloating and gas
- the feeling that you haven’t finished a bowel movement
- whitish mucus in your stool
- cramping
- constipation
- diarrhea
You may also experience a few other symptoms of IBS unrelated to the intestine, including:
- Migraine headaches
- Sleep disturbances
- Anxiety or depression
- Fibromyalgia
- Chronic pelvic pain
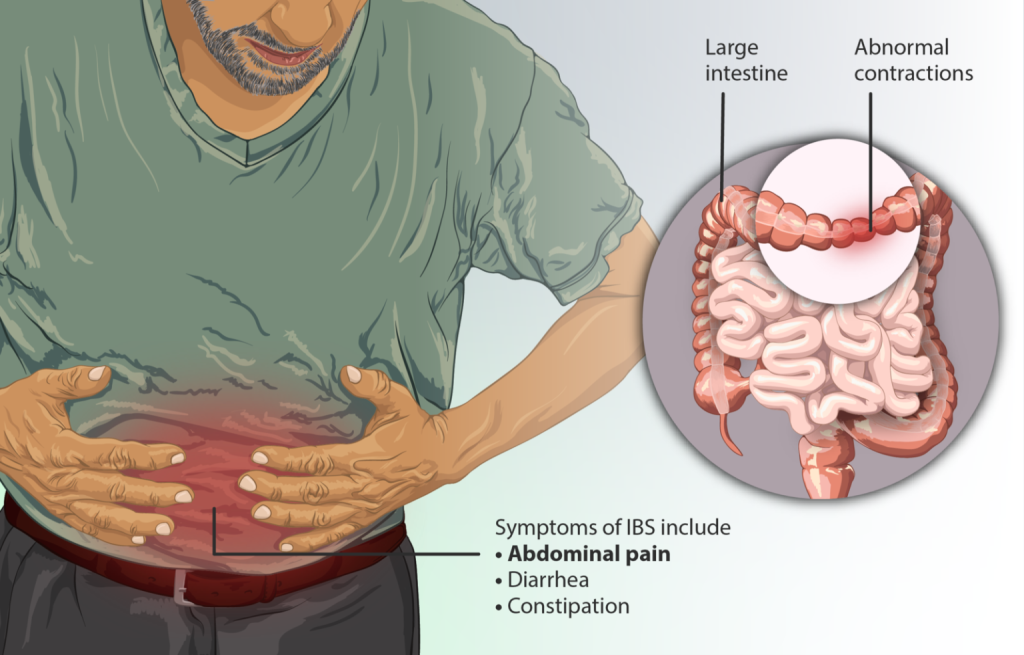
Why IBS happens?
Experts think that a combination of problems may lead to IBS although it’s not clear to date. Hitches in brain-gut axis interaction may control how your body works and cause your digestive tract to work and change how your bowel muscle contract. The result is IBS.
The factors that trigger IBS in you may not be the same as those of your friend
These factors differ from person to person
- If you are young: IBS occurs more frequently in people under age 50.
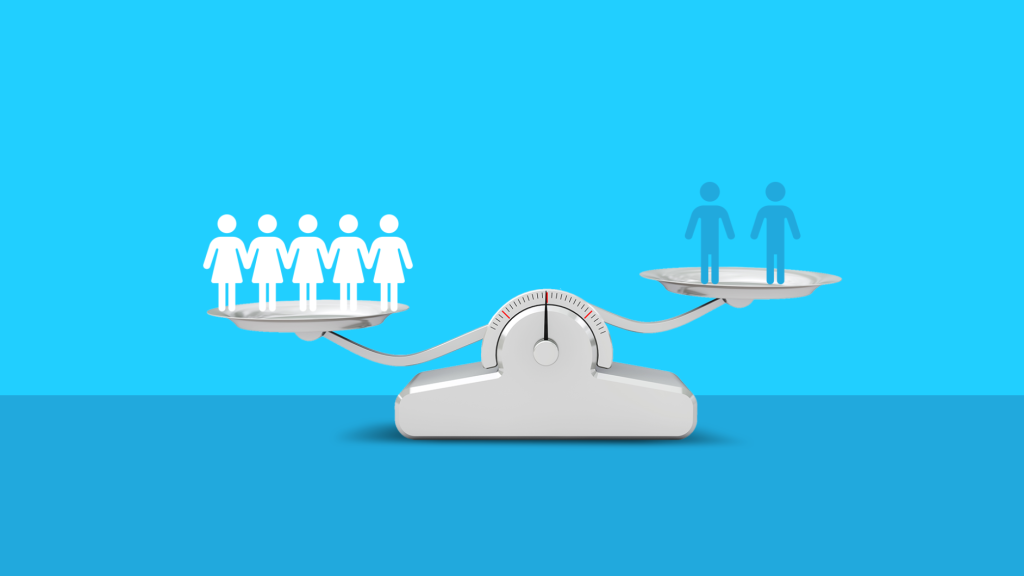
- If you are a female: IBS is more common among women. Estrogen therapy before or after menopause also is a risk factor for IBS.
- If you have a family history of IBS: Genes may play a role, as may share factors in a family’s environment or a combination of genes and environment.
- If you have anxiety, depression or other mental health issues: A history of sexual, physical or emotional abuse in early life events also might be a risk factor.
- If you have any bacterial infection in your gut
- If you have small intestinal bacterial overgrowth: change in their composition and abundance
- If you are intolerant or sensitive to any certain food
Genes may make you more likely to develop IBS
In some cases, a single-gene mutation may promote the genetic risk stems. However, in most cases, the risk is due to polygenes which are genes with individual effects too small to make a noticeable difference, but that can produce a noticeable variation in combination with others.
TNFSF15 gene was reported in different studies to be associated with increased risk of IBS. This gene encodes the TL1A protein expressed in our immune cells, which promotes inflammatory response in the gut mucosa.
Does IBS run in families?
In spite of the genetic ties, research cannot find a strong genetic cause of IBS. It can affect members of the same family, but may be due to shared lifestyles and other risk factors.
There are different types of IBS:
IBS with constipation (IBS-C): when your poop is hard and lumpy
IBS with diarrhea (IBS-D): when your poop is loose and watery
IBS with mixed bowel habits (IBS-M): if you have both hard and lumpy bowel movements and loose and watery movement on the same day
How IBS can be diagnosed?
Doctor may diagnose IBS based on your symptoms and history.
But blood tests, stool tests, and other tests (e.g. hydrogen breath test, upper GI endoscopy with a biopsy, colonoscopy etc.) can help you to check for other health problems (such as iron deficiency anemia, small intestinal bacterial overgrowth, celiac disease, colon cancer or inflammatory bowel disease etc.).
Are there any complications of IBS?
- Poor quality of life: Many people with moderate to severe IBS report poor quality of life.
- Mood disorders: Experiencing the symptoms of IBS can lead to depression or anxiety which also can make IBS worse.
- No risk to develop serious gastrointestinal problems
Can you prevent IBS?
Polyphenols as they have antioxidant and anti-inflammatory properties may help you to protect against heart disease, cancer, diabetes, and gastrointestinal conditions.
Where do you get polyphenols?
Sources of polyphenols include: fruits, vegetables, whole grains, nuts, olive oil, tea, coffee.
Are there any treatments of IBS? What are they?
There is no cure for IBS but to manage problems. No specific therapy works for everyone, your health care provider will personalize your IBS treatment plan for your needs. Typical treatment options include the following:

- Changes in food habits:
- intake of more fibre rich food
- avoiding gluten containing food
- avoiding caffeine, limit milk product as most people with IBS have Lactose intolerance
- following a special eating plan called the low FODMAP diet
- Changes in lifestyle
- increasing your physical activity
- quit smoking
- reducing stressful life situations as much as possible
- getting enough sleep
- Medicines: Different medicines are used to treat IBS with diarrhea, IBS with constipation and abdominal pain. But you should follow your doctor’s instructions when you use medicine to treat IBS.
- Probiotics: These are live microorganisms, most often bacteria, similar to microorganisms you normally have in your digestive tract.

Sometimes doctors may recommend mental health therapies to help improve your IBS symptoms.
There is no cure for IBS but it is not a life threatening disease. Though living with it is challenging as it can come and go throughout your life but there are many personalized treatments to manage it.
Comment
2023-06-23 13:30:23
Mild dose of anxiolytic + probiotics & / or mebevorine helped my mother to get relief from IBS.
Check Your EGFR
***We Promise, no spam!







2023-07-17 07:01:56
Useful