- 1089
- 0
Promising a Thalassemia-Free Future
Thalassemia – A Major Public Health Concern

Picture the excitement of expecting parents, eagerly awaiting the birth of their first child, suddenly confronted with a difficult decision during the fourth month of pregnancy. Their joy turns to heartbreak as they discover that both carry the thalassemia gene, a condition that can pass on to their baby with devastating consequences. This scenario, though distressing, is not rare and often remains undetected until it’s too late.
In a world where many rely on astrology for marriage compatibility, it’s crucial to realize that genetic diseases like thalassemia affect about 7% of the global population, leading to approximately 10,000 thalassemia-affected births in India annually. This urgent reality emphasizes the critical need for genetic screening alongside, or even surpassing, traditional horoscope matching. Prioritizing genetic screening before marriage ensures proactive medical guidance, significantly reducing the risk of such heartbreaking tragedies.
Why Should You Get Tested for Thalassemia?
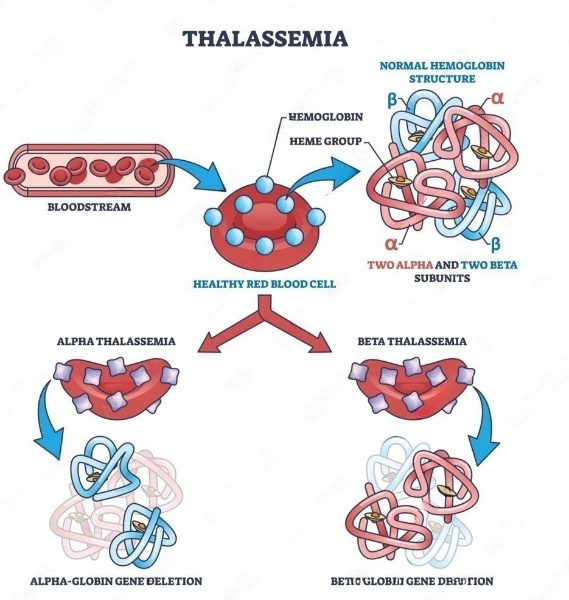
Hemoglobin, essential for healthy blood, has two parts: alpha and beta proteins. When one of these proteins isn’t produced properly, it leads to alpha (α) or beta (β) thalassemia. The severity depends on the type and whether it’s ‘minor,’ ‘intermediate,’ or ‘major’—based on gene alterations. α-thalassemia is more common in certain regions such as India, the Middle East, and Africa, while β-thalassaemia is more prevalent in the Mediterranean.
In India, approximately 42 million individuals carry the β-thalassemia trait, with a higher concentration found among communities such as Sindhis, Punjabis, Gujaratis, Bengalis, Mahars, Kolis, Saraswats, Lohanas, and Gaurs. Notably, in West Bengal and Northeastern states, the Hb E variant of hemoglobin significantly contributes to the prevalence of thalassemia.
You might think that only those with thalassemia minor, intermediate, or major can pass on the disease. However, even without symptoms, you could carry the thalassemia gene. Passing this gene to your children can cause thalassemia, especially if both you and your partner are carriers. Understanding this genetic puzzle is crucial for informed family planning and preventing thalassaemia major.
Understanding Thalassemia: A Genetic Puzzle
Thalassemia is an inherited condition that arises from specific genes passed down from parents, often showing various symptoms within the first two years of life. It disrupts the normal production of red blood cells in the bone marrow, leading to anemia. If left untreated, it can lead to severe medical complications and, in some cases, even death.
Our genetic makeup, consisting of 23 pairs of chromosomes, includes genes responsible for thalassaemia located on chromosome number 11, which is one of the autosomes. The inheritance pattern is recessive, meaning the disease becomes apparent only when both copies of the gene are affected.
Let’s delve into how thalassaemia presents based on our genetic combinations, known as genotypes. For instance, if both parents carry the beta thalassemia minor gene (Hh), there’s a 25% chance of their child having thalassemia major (hh). Alterations or deletions in these genes can disrupt the production of globin chains, leading to the development of thalassaemia. Offspring inherit this disorder from their parents, highlighting the genetic nature of thalassaemia transmission.
Factors related to Thalassemia.
Consanguineous Marriage –marriages that occur between closely related individuals, is an Influential Factor. Currently, one billion of the global population lives in communities with a preference for consanguineous marriage.
So, these kinds of marriages should be prevented to stop the production of thalassemia major children, because the children can die at early age and has been seen to survive maximum up to 15 – 20 years with frequent blood transfusions.
Disease Manifestation and Treatment Burden
The effects of thalassaemia on physical health can lead to physical deformity, growth retardation, and delayed puberty, and this contributes to poor self-image for the patient. Even, children with chronic physical illnesses like thalassemia are prone to get emotional and behavioral problems. The chronicity and complications of thalassemia not only disturb the quality of life of victims but also it hampers the whole family. Children with thalassemia in the pre-school and latency age groups are usually anxious and excessively dependent on their parents.
Screening Test
With early prenatal screening and detection, it is possible to diagnose a congenital defect as early as possible during pregnancy. Screening tests and diagnostic tests are the two types of tests. Prenatal screening is recommended for all expectant mothers.
How is Thalassemia Diagnosed?
A. Blood Tests
The first step in diagnosis usually involves a complete blood count (CBC) to check for anaemia and abnormal red blood cells. If the CBC results suggest that thalassemia might be present, further testing will be done.
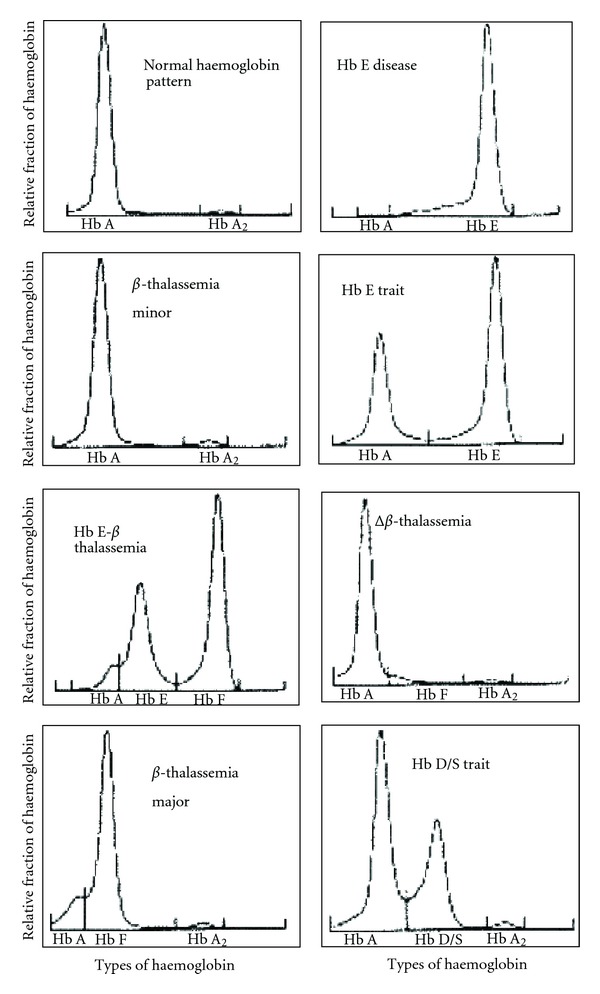
One common blood test used for thalassaemia diagnosis is haemoglobin electrophoresis, which measures the level of different types of haemoglobin in the blood. People with thalassemia have lower levels of normal adult haemoglobin and higher levels of fetal or abnormal haemoglobins.
B. DNA Tests
Another tool for diagnosis is DNA analysis, which can detect mutations in specific genes associated with thalassemia. This test is particularly useful for people who are carriers of the disease and may not show any symptoms but could pass on the disease to their children.
To know more about the urgency of genetic screening in kidney disease CLICK here 👇
In some cases, prenatal testing may also be recommended for couples at risk of having a child with severe forms of thalassaemia. Testing can include chorionic villus sampling (CVS) or amniocentesis to analyze fetal DNA and determine if the baby has inherited the disease.
C. Imaging Tests
X-rays of the bones may be used to detect the bone abnormalities caused by thalassaemia. These X-rays can help with diagnosis and monitor the progression of the disease.
Magnetic resonance imaging (MRI) is used to look for iron overload in the heart, liver, or other organs. Iron overload can damage organs over time and is a common complication of this disease.
Ultrasound is used to measure the size of the spleen and check for other abnormalities in the abdominal area. An enlarged spleen can be a sign of thalassaemia.
For any further enquiry please visit our website or dial to our helpline number +91 806 984 1500
Treatment Options
Treatment for thalassaemia will depend on the type and severity of the condition. Common treatments may include:

- Blood Transfusions: Regular blood transfusions can help reduce anaemia caused by thalassaemia.
- Iron Chelation Therapy: This treatment helps remove extra iron from the body, which often builds up due to frequent blood transfusions.
- Bone Marrow Transplant: Bone marrow or stem cell transplants may be used to treat severe forms of thalassaemia. This procedure involves replacing unhealthy bone marrow with healthy, donor marrow.
Thalassaemia is a big health challenge. Imagine if parents find out they have thalassemia during pregnancy—it’s tough! So, it’s crucial to check for thalassemia genes early on. Getting tested and starting treatment quickly can help manage this disorder. We also need to talk more about things like family history and how thalassemia affects our health and emotions. By doing these things, we can prevent thalassaemia from causing more problems in the future and keep everyone healthier.
References
- Thalassemia patient family studies-Google Search. [Online]. Available from: https://www.google.co.in/?gfe_rd=cr and ei=-3bcWPKbDayo8wf2pL6gAw&gws_rd=ssl#safe=off&q=thalassemia+patient+family+studies&*
- Eiser C. Psychological effects of chronic disease. J Child Psychol Psychiatry. 1990;31:85–98.
- Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: An increasing global health problem. Bull World Health Organ. 2001; 79: 704–712.
- Genetic testing of thalassemia – carrier screening and NIPT. Available from: https://medicover-genetics.com/genetic-testing-of-thalassemia-carrier-screening-and-nipt/
- Thiyagarajan A, Bhattacharya S, Sharma N, Srivastava A, Dhar DK. Need for a universal thalassemia screening programme in India? A public health perspective. J Family Med Prim Care. 2019 May;8(5):1528-1532
- Thalassemia. Available from: https://www.mayoclinic.org/diseases-conditions/thalassemia/diagnosis-treatment/drc-20355001
- Thalassemias. Available from: https://my.clevelandclinic.org/health/diseases/14508-thalassemias
Comment
Check Your EGFR
***We Promise, no spam!